Many benefits of comprehensive genomic profiling (CGP), such as increased throughput, accuracy and therapy precision, are empowering more and more cancer patients to seek matched therapy, and oncologists to seek more comprehensive sequencing solutions.
However, despite steady increases in CGP use, the true role it can play in real-world clinical practice has been largely undefined. Part of this is fueled by questions surrounding CGP’s clinical actionability: Will using this test change how an oncologist treats a patient? Many cite a cardinal rule of diagnostics they learned in medical school: Don’t order a test unless you know how you will use the result.
The lack of a solidified framework to discuss actionability and measure its value in the real world presents a significant barrier to CGP manufacturers promoting its widespread adoption.
Today, CGP’s value is largely characterized by its ability to guide treatment choice for various targeted therapies. Traditionally, a physician suspecting non-small-cell lung cancer in a patient may run an Epidermal Growth Factor Receptor (EGFR) mutation test as per National Comprehensive Cancer Network (NCCN) guidelines. This test would reveal the presence or absence of an EGFR driver mutation in the patient’s genome; if positive, this patient may be prescribed a targeted therapy such as erlotinib, gefitinib, afatinib and osimertinib—typically ahead of chemotherapy or immunotherapy.
CGP, which often charts 50 or more biomarkers, could help shed light on EGFR but it could also provide insight on other non-small-cell lung cancer (NSCLC) biomarkers like ALK, KRAS and ROS1, as well as many other biomarkers that are not targeted by NSCLC treatments today. If the NSCLC biomarkers do not guide a treatment decision, physicians and payers alike may believe that CGP lacks actionability. Unfortunately, this characterization is limited and undermines the complexities of clinical decision-making, especially in oncology. In this frame of thinking, physicians avoid ordering CGP in favor of single-gene or hot-spot panels, and payers become reluctant to cover CGP.
The reality is that the benefits of CGP stretch beyond the ability to match biomarker results to a targeted treatment. Many clinically relevant insights can be drawn from CGP data and a multitude of actions can be taken with these insights: Reframing the definition of actionability is a critical element to shaping the value of this test and ultimately its potential impact on a patient’s cancer.
CGP yields knowledge of an individual’s genomic alterations across multiple stretches of cancer-related genes and across multiple classes of genomic alterations. If present, that knowledge contributes to a holistic yet individualized view of cancer, including:
- Patient categorization: CGP data can contribute to characterizing the patient’s disease or subtype. Any number of biomarkers could help correctly identify the disease subpopulations the patient falls within, and this information can serve as a starting point to guide first-line treatment or identify the next potential therapy.
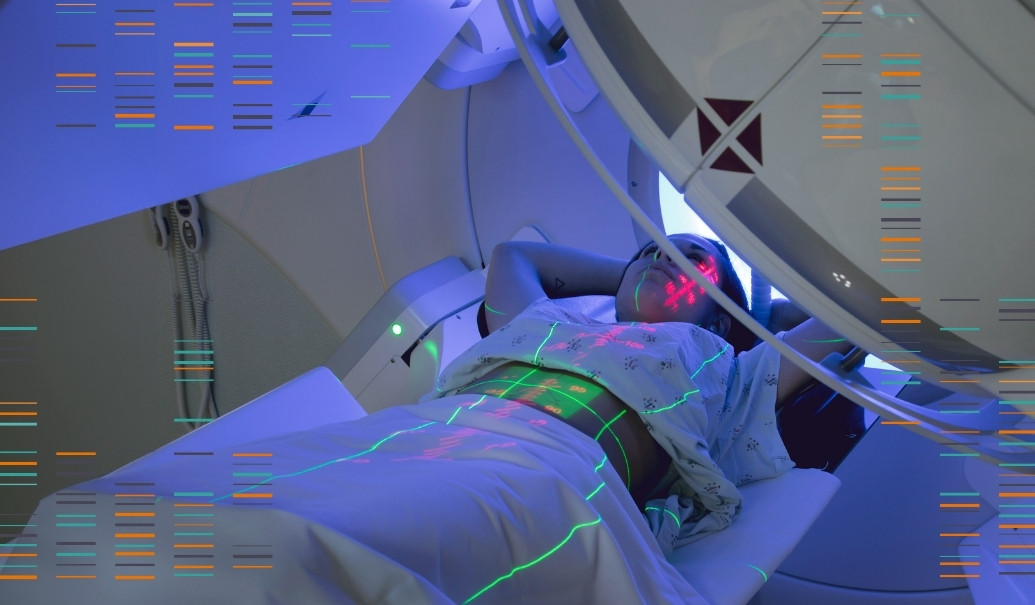
- Determining eligibility for treatment: The presence of a biomarker or lack thereof can direct patients toward the clinical trial for which they are eligible. It may also qualify patients for evidence-based off-label therapy. In other cases, CGP results can also reveal a patient’s sensitivity or resistance to targeted therapy. Simply moving on to, or resuming, standard of care treatments—including chemotherapy, radiation, hormone therapy and nonvariant-directed targeted agents—are also what CGP data can reveal as options.
- Better informing patients about the disease: CGP data can provide general information regarding the patient disease status, such as prognostics and the likely outcome of cancer—risk for progression or overall survival rates and time to treatment failure—for that patient subpopulation. Furthermore, longitudinal studies on patient outcomes conducted in the future will make such information available for certain cancer types where there was previously poor visibility.
- Collect the appropriate evidence to evaluate the risk-benefit profile of particular patient cohorts:
- Refine clinical trial design and improve accuracy of patient matching to biomarkers
- Track longitudinal data on patient outcomes
- Predict process of disease evolution
- Increase concomitance between diagnostics and pharmaceuticals
- Engage KOLs and physicians to help optimize treatment outcomes by analyzing and evaluating clinically relevant CGP data:
- Contribute to growing volume of real-world data and evidence
- Inform candidate selection during drug development
- Advocate for accessibility of CGP at their setting
- Collaborate with payers to enable access to CGP by developing appropriate reimbursement pathways:
- Investigate budget impact of companion or complementary diagnostics
- Conduct cost-effectiveness analysis of predictive biomarkers in reducing costs as well as toxicities associated with ineffective treatments
- Support publication of biomarker coverage guidelines to mediate unfamiliarity with NGS reimbursement
The following steps can enable CGP manufacturers to empower CGP as a universal tool in cancer treatment and ultimately improve cancer care and patients’ lives.
- Understand how physicians and payers define clinical actionability today: Evaluate perceptions among customers to establish a baseline that will determine how significant market development efforts will need to be.
- Identify the drivers and barriers to CGP: For relevant customers, explore the dynamics that influence the tipping point of adoption broadly and personally. This tipping point may be driven by personal comfort or number of approved biomarker-driven therapies, while others may be driven more by accessibility. (For example, community oncology practices may have less accessibility as compared to an academic center with in-house CGP.)
- Redefine clinical actionability: Characterize actionability as the ability of the companion diagnostics tool to provide clinically relevant information that enhances the quality and accuracy of patient care, regardless of the presence of a regulatory link to treatment.
- Gather the evidence: Develop a plan to overcome the barriers by identifying the appropriate messaging and evidence required. For example, manufacturers can explore co-investing or partnering with IDNs or large health systems to create an exchange of data to generate the real-world evidence required. These relationships are often win-win for both parties, assuming the manufacturer has foundational relationships with the most influential systems.
- Translate clinical actionability: Communicate evidence through channels that are most meaningful to each stakeholder (NCCN guidelines, ASCO, major journal publications, etc.). In Europe, ESMO Scale of Clinical Actionability of Molecular Targets has already disseminated guidelines on clinical actionability, though this is primarily focused on treatment and whether a biomarker target is ready for routine use, investigation, hypothetical targeted use or a combination in development.
- Inform the future: Anticipate the opportunity to expand diagnostic technology further, whether to adjacent disease areas or upstream to identify patients who have yet to be diagnosed with cancer.